Next Lesson - The Pelvic Floor
Abstract
- There are many important structures in the external and internal genitalia of the woman. They all have important functions, and it is important to know the anatomical location of the following: labia majora, labia minora, clitoris, vagina, urethral opening, perineum, anus, cervix and fornices.
- The epithelium inside the vagina is stratified squamous and contains glycogen as a substrate for lactobacilli to maintain the low pH of the vagina.
- The cervix is the opening to the uterus and protrudes into the vagina. The external os is the opening that can be seen on speculum examination of the cervix and can have two main physiological appearances (pinpoint os and linear os).
- Cervical eversion occurs when the columnar epithelium that normally occurs on the inside of the cervix is on the outside. This can be as a result of the COCP, normal hormonal change or cervical cancer.
- Cervical cancer is screened for with the smear screening program and vaccinated against (causative organism - Human Papilloma Virus).
- The uterus is the organ that supports pregnancy and creates the vesicouterine and rectouterine pouches. It has two components to the wall, the myometrium (muscular component) and the endometrium (lining).
- The female reproductive tract has three axes: vagina, cervix and uterus. Between these lines exist two angles: the angle of -version is between the axis of the vagina and the axis of the cervix (under 180° = anteverted, over 180° = retroverted), and the angle of -flexion is between the axis of the cervix and the axis of the uterus (under 180°= anteflexed, over 180° = retroflexed).
- The fallopian tube is the tube used to transport the egg from the ovary to the uterus. It has four parts: fimbriae, infundibulum, ampulla and isthmus. Ectopic pregnancies can occur anywhere in the abdomen or pelvis, but commonly occur in the ampulla of the fallopian tubes. Consequences of ectopic pregnancy can be severe, so it is important to consider this in differentials for abdominal pain in fertile women.
- The ovaries store, mature and release egg cells. They are pulled into the pelvis by the gubernaculum but are stopped in their anatomical location by the developing uterus.
- Ovaries have three portions: medulla, cortex and epithelium, and are not covered in visceral peritoneum, meaning that the egg could be released into the peritoneal cavity instead of passing into the fallopian tube. Ovarian cysts, polycystic ovarian syndrome and ovarian tumours are common pathologies of the ovaries.
- The broad ligament is a fold of peritoneum that covers the uterus, fallopian tubes and ovaries. It has three divisions relating to which structure it covers (mesometrium, mesovarium and mesosalpinx), and contains arteries and ligaments (ovarian, round and suspensory).
- The ovarian ligament attaches the ovary to the uterus (a remnant of the gubernaculum), and the suspensory ligament of ovary attached the ovary to the lateral abdominal wall.
- The round ligament is also a remnant of the gubernaculum and connects the labia majora to the uterus.
- The reproductive system is very vascular, containing many arteries and veins. It also has lymphatic drainage related to the embryological point of origin, meaning that the ovaries drain into the para-aortic nodes.
- Female genital mutilation involves damage to the female genitalia for non-therapeutic reasons. There are four types, ranging from jewellery piercings to removal of the clitoris to removal of all external genitalia. There can be far reaching consequences for women, and is illegal in the UK.
Core
The female reproductive tract is made up of the ovaries, fallopian tubes, the uterus and the vagina. It is supported by a number of ligaments and muscles which will also be included in this article.
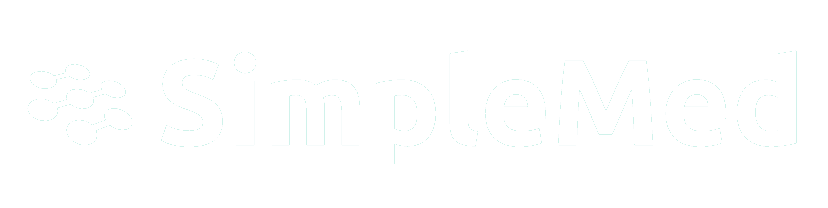
The external genitalia of a woman are comprised of a number of key parts.
Labia Majora – the more prominent folds of tissue that extend from the mons pubis (or pubic symphysis) to the perineum. The labia majora has the same embryological origin as the scrotum in the male (the labioscrotal folds).
Labia Minora – the lesser folds that extend from the clitoral hood to the posterior aspect of the vagina. The labia minora are formed by the urethral folds, which in the absence of testosterone in the female, do not fuse to form the penis.
Clitoris – the glans clitoris is a collection of nerve endings present in the anterior portion of the external genitalia of women. It develops from the genital tubercle (which in males forms the head of the penis) and is covered by the clitoral hood. It is a site of sexual pleasure for most women.
Urethral Opening – the urethral meatus (or opening) is the site through which urine flows out of the body. While it is not part of the reproductive system, it is important to understand its location in relation to other structures of the female genitalia.
Vagina – the vagina is the name for the orifice through which childbirth may occur. It is also the site used commonly in sexual intercourse and the orifice through which menstrual blood flows.
Perineum – this is the portion of skin and muscle that stretches between the vagina and the anus. It is an important structure for the pelvic floor.
Anus – the site of excretion of faeces. Again, not a part of the reproductive tract, but an important anatomical landmark.
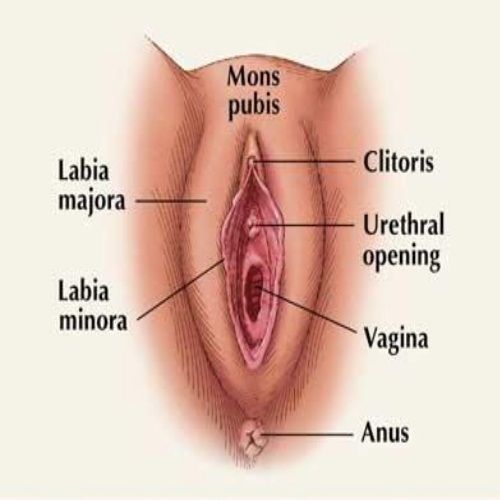
Diagram - External genitalia of the woman
Creative commons source by Sshirly [CC BY-SA 4.0 (https://creativecommons.org/licenses/by-sa/4.0)]
The vagina in humans is a canal that extends from the external genitalia to the cervix in a superior-posterior direction. The urethra and bladder sit anterior to the vagina and the rectum posterior. The vagina facilitates childbirth and intercourse, and due to its muscular walls and rugae (folds in the epithelium), can expand drastically.
At the superior aspect of the vagina lies the cervix. The cervix protrudes into the vagina, leaving a circular gutter between the walls of the vagina and the cervix. This is called a fornix (plural fornices), and can be split into the anterior, posterior, left and right fornix. The fornices can be difficult to see on examination of the vagina and could lead to pathology being missed. The fornices are also the site at which some vaginal swabs are taken.
In the fetus, the vagina develops from the urogenital sinus and the Mullerian Duct (an embryological duct that goes on to form the Fallopian tubes, uterus and vagina).
The vagina is supported by the muscles of the pelvic floor (see below).
The epithelium found in the vagina is a stratified squamous epithelium. The epithelium is relatively glycogen rich and acts to provide a source of nutrition for the lactobacilli that exist naturally inside the vagina. The lactobacilli metabolise the glycogen into lactic acid which creates and maintains an acidic (low pH) environment in the vagina. This low pH helps to inhibit the growth of microorganisms such as Candida albicans (the causative organism of thrush). Practices to ‘clean’ the vagina such as douching can disrupt the pH balance and increase the likelihood of infections like thrush, and so are not advised by clinicians.
The cervix is the opening to the uterus. It is a narrow channel that connects the vagina to the uterus, with the external os being the opening to the vagina, and the internal os being the opening to the uterus. During childbirth, the cervix stretches from the ‘pinpoint’ seen normally on the external os to approximately 10cm wide to allow the baby through. Following childbirth, the external os does not return to the ‘pinpoint’ seen pre-childbirth. This means the external os of women who have given birth will appear more linear in shape (this is normal).
The cervix can also exhibit signs of cervical ectropion. This occurs when the columnar epithelium of the inside of the cervix is shown externally. This can occur as a side effect of taking the combined oral contraceptive pill but is also a normal process linked to hormonal changes.
Diagram - The different appearances of the cervix. It is important to note that normal has more than one form depending on whether childbirth has occurred. The third figure shows cervical ectropion, where the columnar epithelium that is normally inside the cervix is on the outside seen as the red transformation zone
SimpleMed original by Maddie Swannack
There are around 3200 new cervical cancer cases in the UK every year, which is approximately equivalent to 9 diagnoses per day. 63% of women diagnosed with cervical cancer survive 10 years. (source: Cancer Research UK).
Many of these cases are related to two strains of Human Papilloma Virus (HPV strains 16 and 18). HPV is a virus that is sexually transmitted, and causes no symptoms. This means that a woman who is infected with HPV will have a higher chance of developing cervical cancer without knowing it. A vaccine for HPV was introduced in the UK for girls aged 12-13 in 2008, and in 2019, was extended to include boys of the same age (because HPV also increases the risk of anal and penile cancers).
Cervical cancer often does not have any signs until it has developed. Bleeding from the tumour then manifests with bleeding between periods (intermenstrual bleeding), bleeding after sex (post-coital bleeding) and bleeding after periods have naturally ended (post-menopausal bleeding).
The majority of cases of cervical cancer in the UK are diagnosed before presentation through the cervical cancer screening program. Screening is offered to women between 25 and 49 every 3 years, and women 50 to 64 every 5 years. This is because cervical cancer is most common in the sexually active between 25 and 40. The process of cervical screening involves inserting a speculum into the vagina and using a small, brush instrument to take a scraping of cells from the inside of the cervix. This sample is then screened for HPV and the cells are examined to identify any pre-cancerous changes.
The uterus is the reproductive organ of the female that is responsible for supporting pregnancy. It lies in the pelvis superior to the vagina, posterosuperior to the bladder and anterior to the rectum. The potential space between the bladder and the uterus is called the vesicouterine pouch. The potential space between the uterus and the rectum is called the rectouterine pouch or pouch of Douglas. These are important anatomical landmarks because any free fluid in the peritoneum will settle in the pouch of Douglas. Superolateral to the uterus sit the ovaries, connected to the uterus via the Fallopian tubes.
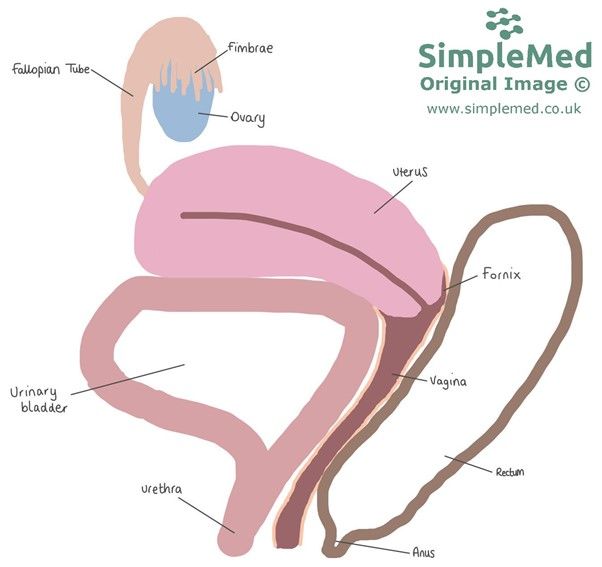
Diagram - The relationship between the vagina, uterus, bladder and rectum
SimpleMed original by Maddie Swannack
The uterus has two components to its wall:
- The myometrium is the muscular component of the uterine wall. It is the muscle that contracts during childbirth and on the shedding of the uterine lining in a menstrual period. This is the source of labour pains and period cramps.
- The endometrium is the epithelial lining of the uterus. During the menstrual cycle the endometrium will proliferate, forming the lining of the womb for the potential embryo to embed in. The endometrium contains a number of glands that change shape throughout the cycle: initially they are straight, then become coiled and secrete glycogen during ovulation, then lose their structure to prompt menstruation. The endometrium is further divided into two sections:
- The functional layer is the layer that sheds during menstruation.
- The basal layer is the static layer that allows proliferation during the next menstrual cycle.
The female reproductive tract is said to have three axis: the axis of vagina, the axis of cervix and the axis of uterine body. These are lines that are drawn onto the anatomy of a woman to describe the general direction that the structure points in.
Between these three lines exist two angles, which are maintained by the round ligament (see later):
- The angle of -version exists between the axis of the vagina and the axis of the cervix.
- If this angle is under 180°, the cervix is said to be anteverted.
- If this angle is over 180°, the cervix is said to be retroverted.
- The angle of -flexion exists between the axis of the cervix and the axis of the uterus.
- If this angle is under 180°, the uterus is said to be anteflexed.
- If this angle is over 180°, the uterus is said to be retroflexed.
It is possible to have any combination of these, as shown in the diagram below. The commonest position is that of anteflexed anteverted.
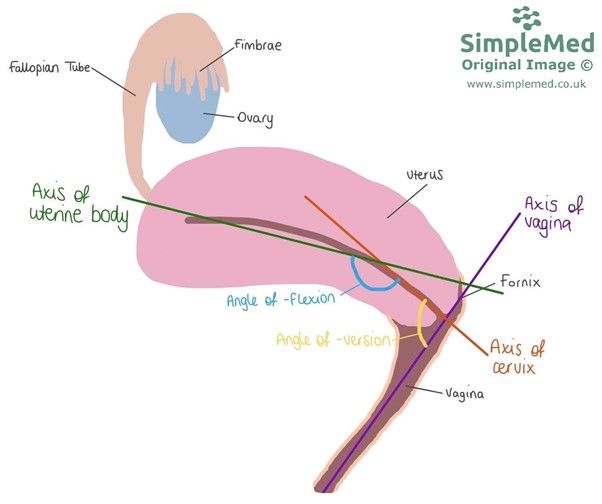
Diagram - The three axes and two angles that exist in the internal female reproductive tract. The angle is said to be an average of the direction (meaning it is a straight line that represents the direction)
SimpleMed original by Maddie Swannack
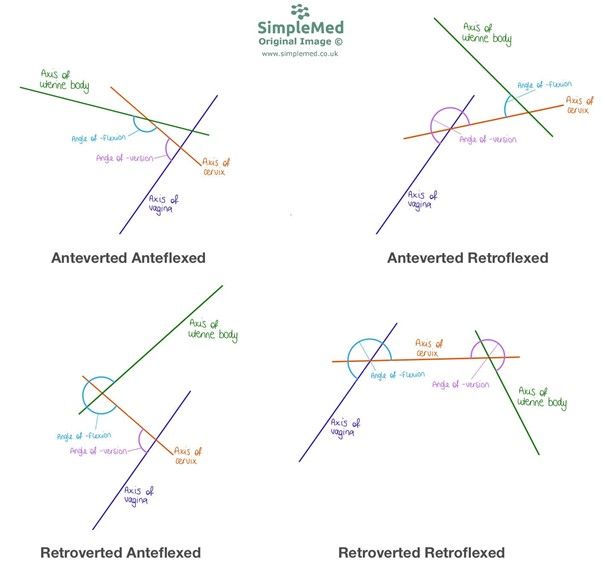
Diagram - The shapes that can be formed by the axis of the internal reproductive tract. While they are all variants of normal, retroversion and retroflexion are rarer, and can cause issues like pain in pregnancy
SimpleMed original by Maddie Swannack
The fallopian tubes transport the egg cell released from the ovary to the uterus and to transport sperm from the uterus to meet the released egg for fertilisation. The tubes are muscular, and contract by peristalsis to encourage the egg towards the uterus. They are also lined with tiny ‘hairs’ that help to waft the egg toward the uterus and the sperm towards the ovary.
The tubes are not attached to the ovary (as shown in the diagram below), which means that the egg could technically be released from the ovary and not make it into the fallopian tube, but instead embed elsewhere in the abdomen. Furthermore, this gap is the only anatomical hole in the peritoneum so can be a source for air and cause a pneumoperitoneum although this is very rare.
There are 4 parts to the fallopian tube:
- Fimbriae – finger like projections that face the ovary that act as a funnel to make sure the egg ends up in the fallopian tube.
- Infundibulum – the first part of the fallopian tube that the egg will enter.
- Ampulla – this word means ‘jug’ and describes the shape of the ampulla (supposedly). It is the middle part of the fallopian tube. It is the most common site of ectopic pregnancy.
- Isthmus – this is the final part of the fallopian tube and is the point of attachment to the uterus.
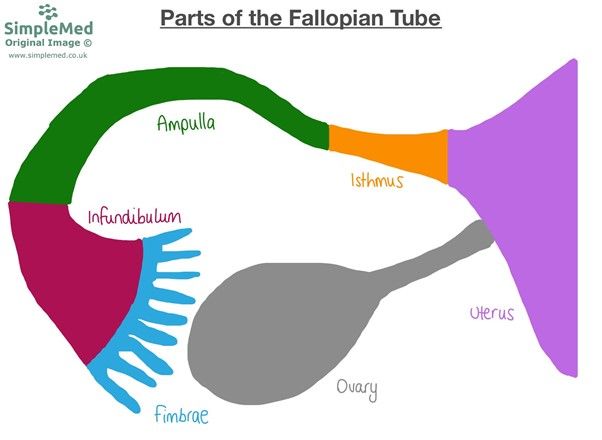
Diagram - The anatomy of the fallopain tubes
SimpleMed original by Maddie Swannack
An ectopic pregnancy occurs when the embryo implants in a position that it is not supposed to, that is other than in the uterus. This can be anywhere but is most commonly in the fallopian tube at the ampulla.
Obviously, the thin fallopian tube is not equipped to grow a fetus, so as the embryo implants in the wall of the fallopian tube and begins to grow, it can rupture the tube causing severe internal bleeding. However, this may not happen until the embryo has grown, meaning it might not rupture until 8-12 weeks.
Initially, ectopic pregnancy might present with vague symptoms like abdominal pain and vaginal bleeding, but it is common for no signs or symptoms to manifest. Once rupture has occurred, pain is very common, and the bleeding can rapidly lead to shock, hypotension and tachycardia. Ectopic pregnancy can also present with shoulder tip pain due to blood irritating the diaphragm causing referred pain in the dermatome of the phrenic nerve roots (C2, C3, and C4).
Consequences of ruptured ectopic pregnancy can be severe. Damage to the fallopian tube is often not recoverable, leading to difficulty in future conceptions and an increased risk of recurrent ectopic pregnancies. It also normally leads to loss of the embryo and can also lead to the death of the mother if the internal bleeding is severe or untreated.
Because ectopic pregnancy is so severe and rapidly life threatening it is an emergency and should be ruled out in any female of childbearing age (approx. 13-50 years old) who presents with abdominal pain. This is routinely done through a pregnancy test (β-hCG) or ultrasound scan.
The gonads in the female are called the ovaries. The ovaries act as the storage and maturation site for the oocyte (egg cell) and act to produce oestrogen and progesterone under the influence of pituitary gonadotrophins; luteinising hormone (LH) and follicle stimulating hormone (FSH).
Like the testicles, the ovaries develop from the mesonephric ridge and descend through the abdomen under the pull of the gubernaculum. However, unlike the testicles, the ovaries stop their descent in the pelvis because the developing uterus gets in the way.
There are three main parts in the ovary:
- Medulla – the medulla is the inner part of the ovary and is the site of neurovascular structures inside the ovary. Its function is to supply nutrients through the blood to the cortex.
- Cortex – the cortex is the outer park of the ovary and is largely composed of connective tissue called stroma. Within the stroma are thousands of follicles (an oocyte surrounded by a layer of follicular cells).
- Epithelium – the epithelial covering of the ovary is made up of germinal epithelium, a form of simple cuboidal epithelium. It is called germinal because it protects the germ cells (in this case egg cells).
It is also important to note that the ovaries are not covered by the visceral peritoneum like the rest of the organs in the abdomen. The visceral peritoneum surrounds the fallopian tubes, but not the ovaries (see drawing below for explanation). This means that technically an egg could miss the fallopian tube, and as the ovaries are not encased in peritoneum, this egg would be released into the peritoneal cavity. This can be dangerous because it can be a site of ectopic pregnancy (if the embryo implants in the peritoneal cavity rather than in the uterus).
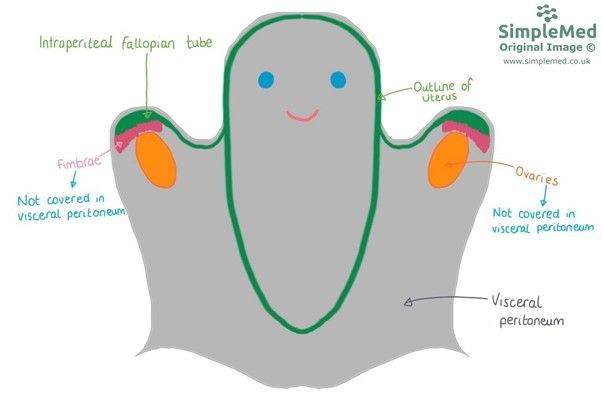
Diagram - A cartoon of the visceral peritoneal coverings of the female internal reproductive organs. It shows how the uterus and most of the fallopian tubes are covered by the visceral peritoneum. It also shows how the ovaries (shown in orange) and the fimbriae of the fallopian tubes (shown in pink) are not covered by the visceral peritoneum, and so exist inside the peritoneal cavity (because the parietal peritoneum is still adhered to the abdominal wall)
SimpleMed original by Maddie Swannack
Ovarian Cysts – cysts can form on the ovaries and are most commonly under 2.5cm in size. Most are benign, and develop while a woman is having regular periods, but some larger cysts can cause problems such as pain or bleeding, and may need surgical removal.
Polycystic Ovarian Syndrome (PCOS) – PCOS is a syndrome of hormonal disturbance characterised by irregular periods (indicating irregular ovulation), excess androgens like testosterone (characterised by hirsutism – excess body hair) and a large number of ovarian cysts. It is associated with infertility.
Ovarian Tumours – most commonly the tumours of the ovaries are epithelial in origin (ovarian adenocarcinoma), but tumours can also be derived from germ cells, which could become any tissue (called teratomas). This means that teratomas can sometimes be made up of lots of cell types and may include hair or teeth (mature teratoma). In women, mature teratomas are benign whereas immature teratomas may spread.
The broad ligament is a flat sheet of peritoneum that covers the uterus, fallopian tubes and ovaries. It is wide (hence its name as the ‘broad’ ligament) and runs from the pelvic wall across the internal genitalia and attaches to the other pelvic wall.
It has three divisions:
- Mesometrium – this portion surrounds the uterus and the external iliac vessels. It also encloses the proximal part of the round ligament of the uterus.
- Mesovarium – this portion is associated with the ovaries. It projects from the broad ligament and attaches to the hilum of the ovary, enclosing the neurovascular bundle that supplies the ovary. It does not enclose the ovary.
- Mesosalpinx – this portion is very small and only covers the fallopian tube.
The broad ligament contains many structures:
- The ovarian and uterine arteries
- The ovarian ligament
- The round ligament of uterus
- The suspensory ligament of ovary (also known as the infundibulopelvic ligament)
Ligaments Associated with the Ovary
There are two main ligaments that attach to the ovary.
Ovarian Ligament – the ovarian ligament attaches the ovary to the uterus. It is a fibrous band that lies within the broad ligament and joins the uterus just inferior to where the fallopian tubes join. The ovarian ligament is a remnant of the gubernaculum in the female. The round ligament of the uterus makes up the rest of the old gubernaculum and attaches the uterus to the labia.
Suspensory Ligament of Ovary – the suspensory ligament of ovary extends outwards from the ovary to the lateral abdominal wall. It is a fold of the peritoneum but is normally considered to be separate to the broad ligament. It contains the ovarian artery, vein, nerve plexus and lymphatics. It is also known as the infundibulopelvic ligament.
Ligaments Associated with the Uterus
There are several ligamentous structures that attach to the uterus. They can be classified by where they attach to the uterus:
- Superior – broad ligament and the round ligament.
- Inferior – pelvic floor muscles like levator ani and the perineum.
Round Ligament – the round ligament is the remnant of the gubernaculum, which is the fibrous band that guides the ovaries towards the labia. It therefore attaches to the labia majora, passes through the inguinal canal, and attaches to the uterus at the point that the fallopian tubes also join. In pregnancy, the round ligament can be a source of pain due to the increased force placed on the ligament by the expanding uterus.
The gubernaculum is the structure that draws the gonads towards the labioscrotal folds. In males, this guides the testicles into the scrotum. In females, this guides the ovaries towards the labia majora. However, in the female, the developing uterus stops this path, causing the ovaries to remain in the pelvis. This means that the gubernaculum runs from the ovaries to the uterus to the labia majora, forming the ligament of ovary and the round ligament.
The reproductive system of the female is a very vascular structure.
The main arteries are the ovarian artery and the uterine artery, which anastomose across the uterus creating the Helicine branches. They also branch to form the tubal vessels, which supply the fallopian tubes. The uterine artery is a branch of the internal iliac artery, but the ovarian arteries arise directly from the abdominal aorta.
The vagina is supplied by the vaginal arteries which are also branches of the internal iliac arteries.
Venous drainage of the ovaries is achieved by the ovarian veins. The left ovarian vein drains into the left renal vein which then joins the inferior vena cava. The right ovarian vein drains directly into the inferior vena cava.
The uterus drains into the uterine veins via a plexus in the broad ligament. The vagina also drains via a plexus into the vaginal vein. Both then drain into the internal iliac vein.
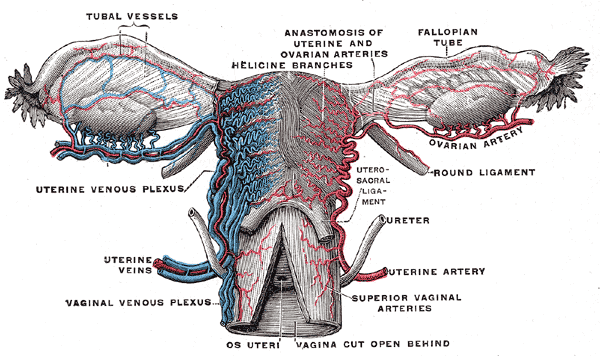
Diagram - The vascular supply of the female reproductive system
Public Domain Source by Henry Gray: Gray's Anatomy (20th edition) [Public domain]
The lymphatic drainage of the ovaries is positioned relating to their embryological position in the upper abdomen (before their descent into the pelvis). This means they drain into the para-aortic nodes. This is important because it means that cancer of the ovaries may spread to the para-aortic lymph nodes first.
The lymphatic drainage of the uterus includes the iliac, sacral and inguinal lymph nodes, and the vagina drains into the iliac and inguinal nodes.
Female genital mutilation (or FGM) includes any procedure involving the removal of or injury to the external female genitalia for non-therapeutic indications. It is a practice that is more common in the culture of certain African nations but that has worldwide implications through global migration and culture.
There are 4 types:
- Partial or total removal of the clitoris.
- Partial or total removal of the clitoris and labia minora.
- Narrowing of the vaginal orifice with the creation of a covering seal by cutting and appositioning the labia, and then stitching them together.
- All other harmful procedures including piercing, cutting and cauterising.
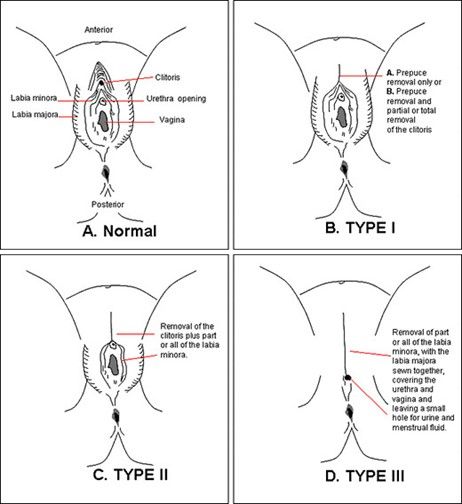
Diagram - Three of the four types of FGM. Type 4 includes any type of piercing including with jewellery
Public Domain Source by Blatant World [Public domain]
Acute Consequences – haemorrhage, sepsis, HIV or hepatitis infection (from instruments that have not been sterilised) and death.
Chronic Consequences – difficulties during sex or childbirth, chronic pain, obstructive dysmenorrhoea (difficulty menstruating), urinary outflow obstruction and PTSD.
Legality
FGM is illegal in the UK, and performing it carries a prison sentence of up to 14 years. It is also illegal to return the genitalia to its previous appearance after damage (e.g. in childbirth), even if requested to do so by the patient.
Healthcare professionals have a legal duty to report occurrence of FGM in any person under 18, and to offer support to women over 18 who show it.
Edited by: Dr. Ben Appleby and Dr. Thomas Burnell
- 8038